Differences among Nursing Homes in the Outcomes of a Safe Resident Handling Program
07/26/2013
By Alicia Kurowski, Sc.D., Post-Doctoral Fellow, CPH-NEW, UMass Lowell
Issue #32
Differences Among Nursing Homes in the Outcomes of a Safe Resident Handling Program, CPH News and Views, Issue #32
Healthcare workers are known to have high rates of low-back and other musculoskeletal injuries, often related to handling patients or residents. Safe Resident Handling Programs (SRHP) in long-term care can reduce workers’ physical workload and injury risk. The CPH-NEW “ProCare” study evaluated a SRHP by observing nursing assistants (NAs) in five nursing homes while they worked. We recorded information about body postures and resident handling activities before the SRHP began (“baseline”) and then 3 months, 12 months, and 24 months later. These observations were used to determine changes over time in the use of resident handling equipment and in NAs’ physical workload. We also examined factors that might predict differences among centers in program effectiveness. [1]
Safe Resident Handling Program Outcomes
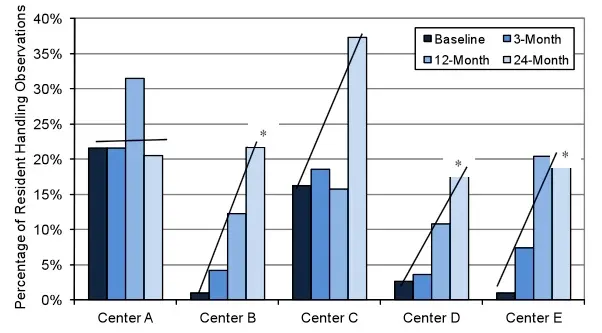 Equipment use (Total Body Lifts, Sit-to-Stand Lifts, Slideboards, Slipsheets, and Gaitbelts) while resident handling increased over time, especially among the centers with little or no equipment in use at baseline.
Equipment use (Total Body Lifts, Sit-to-Stand Lifts, Slideboards, Slipsheets, and Gaitbelts) while resident handling increased over time, especially among the centers with little or no equipment in use at baseline.
- Equipment use increased the most at centers B, D, and E.
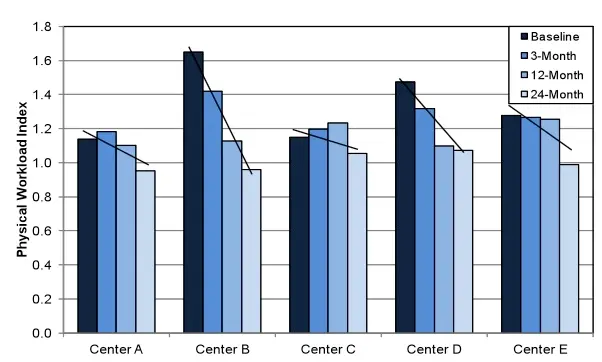 Physical workload, from the combination of awkward body postures and weight in the hands during resident handling and other tasks, decreased among NA’s over the two years that we observed them.
Physical workload, from the combination of awkward body postures and weight in the hands during resident handling and other tasks, decreased among NA’s over the two years that we observed them.
- Physical workload decreased most at centers B, D, and E.
Differences among Centers
Based on firsthand experience while making observations, we developed a list of factors that might lead to differences among centers in SRH equipment use. Information on explanatory factors was extracted from administrative records, employee satisfaction surveys, observations, and post-observation interviews. Factors were tested for correlation with change in equipment use and change in physical workload over two years.
Factors associated with center differences
Over two years, equipment use increased more in the centers with low NA turnover, low administrator turnover, few perceived obstacles to getting work done on time, and low feeling of time pressure among NA’s. Physical workload decreased more in centers with improvements in staff ratings of staff-to-staff communication, quality of teamwork, and adequacy of supplies.
Conclusions and Recommendations
In the five centers where we observed CNAs working, it appears that use of resident handling equipment reduced their total physical workload, as intended. However, the benefits were more impressive in some centers than others. Those with bigger improvements had better work environments in many other ways, such as less time pressure, fewer shifts with obstacles to getting work done on time, better staff communication, and better access to supplies.
- Routine equipment maintenance schedules can improve access to handling equipment, reduce obstacles to getting work done on time, and relieve time pressure for NAs.
- Training to encourage open communication and teamwork between NAs and their supervisors, as well as among NAs themselves, can reduce health and safety risks.
- Limiting understaffing situations can relieve time pressure among NAs, and reduce exposure to excessive physical workload.
The bottom line
Safe resident/patient handling programs are economically beneficial in health care settings. Increased equipment use and decreased physical workload for nursing personnel can lead to reductions in lost injury days and workers’ compensation claim costs.[2] In addition, improving the social and psychological work environment in the ways suggested above may help mitigate turnover.[3] Retention of highly trained staff who work together well and are competent users of handling equipment is in the best interests of all involved. On average, yearly turnover in U.S. nursing homes is 75% for NA’s, 56% for RN’s, and 51% for LPN’s. The ratio of turnover costs to annual wages is about 1.0 for RNs and 0.25 for other clinical staff, so this represents high costs for health care facilities. The human asset – A nursing home that invests in a SRHP is investing in the health of the employees, thus showing respect for their health and their work.
References:
- Kurowski, A., Gore, R., Buchholz, B., Punnett, L., 2012. Differences among nursing homes in outcomes of a safe resident handling program. Journal of Healthcare Risk Management, 32(1):35-51.
- Lahiri S, Latif S, Punnett L, ProCare Research Team. An economic analysis of a safe resident handling program in nursing homes. Amer. Journal of Industrial Medicine 2013; 56(4):469-78.
- Zhang Y, Punnett L, Gore R. Relationships among employees' working conditions, mental health and intention to leave in nursing homes. Journal of Applied Gerontology. [E-pub 23 April 2012.].
CPH-NEW is a Center for Excellence to Promote a Healthier Workforce of the National Institute for Occupational Safety and Health. CPH-News & Views is a semi-monthly column written by Center researchers on emerging topics related to healthy workplaces. These comments reflect thoughts of the individual researchers and do not represent conclusive research summaries, nor do they necessarily reflect a consensus among all Center personnel. We welcome your responses and discussion. Please send all questions and comments to CPHNEW@uml.edu.
CPH News and Views Issue 32
© Copyright 2013 The Center for the Promotion of Health in the New England Workplace (CPH-NEW)
July 2013
