Minding the Gap Between Research and Practice
06/20/2014
By Alicia Dugan, PhD, Assistant Professor, University of Connecticut Health Center
Issue #37 (pdf)
Minding the Gap between Research and Practice: Can we predict which organizations and people will most successfully implement a health-oriented innovation?
“If you build it, they will come.” This quote from the movie, “Field of Dreams,” summarizes the long-standing attitude of researchers toward their “evidence-based health innovations” (EBHIs), meaning interventions that have been shown scientifically to have health benefits. It seems logical that programs, practices, and policies with proven efficacy to prevent or treat illness would enjoy widespread uptake in real-world settings, but in fact this is not the case.
Public health scientists now realize that some efficacious and cost-effective interventions (e.g., water-boiling to prevent infection in Peruvian villages) [Rogers, 2003] have failed miserably to be adopted into practice, while other “health interventions” with no established efficacy have been extraordinarily successful in being widely adopted (e.g., the Paleo diet, one of the most popular diets of 2014 [McMullen, 2014]. Despite billions of dollars spent worldwide on the development of EBHIs, only a small portion are ever translated into practice - and when they are, it takes an average of 17 years [Balas & Boren, 2000; Grol, 2007].
What do we need besides evidence of effectiveness?
If efficacy alone is not compelling enough, what factors do help ensure that EBHIs get adopted widely in clinics and communities? A new and growing field of research known as “Dissemination and Implementation (D&I) Science” is dedicated to answering this question. Its mission is to narrow the gap between research and practice by identifying and addressing both the barriers and facilitators of EBHI adoption and spread.
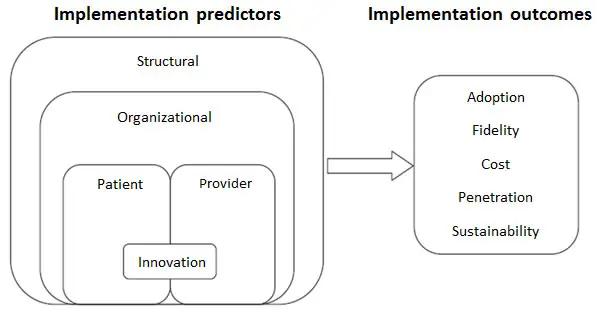 The challenge is that, like snowflakes, each instance of EBHI implementation is unique, unrepeatable in all details and therefore difficult to compare to other implementation efforts. The EBHI goals, general context, and specific people involved all introduce variability. The good news is that there are useful frameworks to identify barriers and facilitators of successful EBHI implementation. One such framework, at right [Chaudoir et al., 2013], identifies a set of important concepts that cover all of the “moving parts” associated with EBHI implementation. It is comprehensive, in that it considers both predictors and outcomes of implementation, and it applies to a wide range of EBHIs and contexts where these might be adopted.
The challenge is that, like snowflakes, each instance of EBHI implementation is unique, unrepeatable in all details and therefore difficult to compare to other implementation efforts. The EBHI goals, general context, and specific people involved all introduce variability. The good news is that there are useful frameworks to identify barriers and facilitators of successful EBHI implementation. One such framework, at right [Chaudoir et al., 2013], identifies a set of important concepts that cover all of the “moving parts” associated with EBHI implementation. It is comprehensive, in that it considers both predictors and outcomes of implementation, and it applies to a wide range of EBHIs and contexts where these might be adopted.
What predicts implementation success? How can we tell if we’ve been successful?
According to the Chaudoir framework, implementation predictors are variables that can either enable or obstruct implementation success. They fall within one of five nested levels (see the left side of the diagram above). The structural level refers to characteristics of the larger social-cultural context where the implementing organization is located (for example, a community that is politically liberal or conservative, rural or urban). Within that, aspects of the specific organization may either help or interfere with implementing the EBHI (for example, supportive leadership or a culture of innovation). Provider-level variables are characteristics of the person implementing the EBHI (for example, knowledge level or degree of self-confidence). Patient-level or employee-level variables are characteristics of the person who would expect to benefit from the program (for example, their gender, age, or readiness to change health behaviors). Finally, innovation characteristics are aspects of the EBHI itself that increase the likelihood of uptake or implementation (for example, its adaptability or ease of use).
This framework also shows possible implementation outcomes, which are indicators of implementation success: adoption, fidelity (implementing as intended), cost, penetration (reach to all possible recipients), and sustainability (institutionalized into permanent operations) [Proctor et al., 2011]. Generally speaking, implementation efforts can be considered a success if the EBHI is adopted by an organization, was implemented with fidelity, and has a high level of penetration and sustainability.
By applying this framework, researchers and practitioners have a powerful tool for identifying and addressing factors that can promote successful translation of EBHIs into practice, and also to improve the EBHI design and process in future efforts.(*) Although D&I science is still an emerging field of research, it already offers highly useful guidance to understand, and ultimately to start narrowing, the research-to-practice gap.
* Note: Both predictors and outcomes can be assessed qualitatively (e.g., focus groups or interviews) or quantitatively (e.g., survey scales). Chaudoir et al. identified 62 survey measures that have been used to measure predictor variables at all five levels. Proctor et al. discussed outcome variables and measures.
Alicia Dugan, PhD, is an industrial/organizational psychologist who specializes in translational research; she co-authored the article with Chaudoir on D&I measures for health innovations.
References:
- Balas EA, Boren SA: Managing clinical knowledge for health care improvement. In Yearbook of medical informatics 2000: Patient-centered systems. Edited by Bemmel J, McCray AT. Stuttgart, Germany: Schattauer; 2000: 65–70.
- Chaudoir S, Dugan A, Barr C: Measuring factors affecting implementation of health innovations: A systematic review of measures. Implementation Science 2013: 22.
- Grol R, Bosch M, Hulscher M, Eccles M, Wensing M: Planning and studying improvement in patient care: The use of theoretical perspectives. Milbank Q2007,85: 93–138.
- McMullen L: U.S. News Ranks Best Diets for Weight Loss, Healthy Eating, More. US News and World Reports 2014. (Retrieved from http://health.usnews.com/health-news/health-wellness/articles/2014/01/07/us-news-ranks-best-diets-for-weight-loss-healthy-eating-and-more).
- Proctor E, Silmere H, Raghavan R, Hovmand P, Aarons G, Bunger A, Griffey R, Hensley M:Outcomes for implementation research: Conceptual distinctions, measurement challenges, and research agenda. Adm Policy Ment Hlth 2011, 38: 65–76.
- Rogers EM: Diffusion of innovations 5th edn. New York: Free Press; 2003.
