Northeast Rehab Hosts Mini-Conference on Interprofessional Collaboration During COVID-19
 Image by Adrien Bisson
Image by Adrien Bisson
04/26/2021
By Katharine Webster
If a doctor had a spare moment at the end of visiting a COVID-19 patient, she emptied the trash. Physical therapists changed bedsheets. Nurses removed food trays.
Taking care of ordinary housekeeping tasks was just one of the ways that Northeast Rehabilitation Hospital health care professionals adapted to protect each other and their patients while caring for people with COVID-19, nearly 130 physical therapy and nutritional science students learned during a virtual mini-conference on interprofessional collaboration.
“The lines were blurred between roles – from the physiatrist all the way to janitorial staff,” says second-year Doctor of Physical Therapy student Rachel Seeley ’19.
“The doctor said sometimes she would be doing bed mobility with patients, which is our role in physical therapy. Physical therapists were helping with speech therapy, or they would work on the patient sitting at the edge of the bed so the patient could increase their sitting tolerance for eating and swallowing,” Seeley says. “They maximized their creativity so they could have as few people having contact with the patients as possible.”
The mini-conference was the idea of Assoc. Teaching Prof. JoAnn Moriarty-Baron, who teaches Neurological Physical Therapy, a course for second-year doctor of physical therapy students, and Keith Poulin ’07, director of in-patient rehabilitation at Northeast Rehab’s hospital in Salem, New Hampshire.
Moriarty-Baron, who has worked as a clinical mentor and per diem therapist at Northeast Rehab, normally takes her students to visit the hospital so that they can see an acute, in-patient rehab facility and better understand what it’s like to do physical therapy on someone who is neurologically impaired.
“A rehab hospital is a whole different experience” from an outpatient physical therapy clinic, Moriarty-Baron says. “Most students haven’t been exposed to people who’ve had a traumatic brain injury or other neurological injuries.”
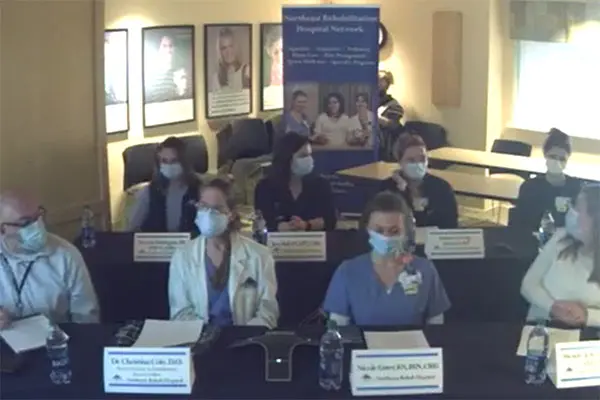 Image by Courtesy
Image by Courtesy
Moriarty-Baron was already working with Poulin, who had put together video case studies of stroke patients for use in her remote classes during the pandemic, when they came up with the idea for the mini-conference. Northeast Rehab, which employs many UML alumni, also accepts many physical therapy students for clinical rotations.
Last month, Poulin gathered with seven colleagues in a single room, including a doctor, a physical therapist, a nurse, an occupational therapist, a speech pathologist, the nutrition manager and the COVID unit manager.
With a camera trained on them so that students could see them on Zoom, they talked about the challenges and rewards of their work when they agreed to take COVID-19 patients during the pandemic’s first surge in spring 2020 – and then again in November, when an outbreak among patients and a second surge required them to re-establish a COVID unit.
Students in Moriarty-Baron’s course and a graduate Cardiopulmonary Physical Therapy I class, along with undergraduate nutritional science majors taking Life Cycle Nutrition and Medical Nutrition Therapy, watched it live. They submitted questions in advance, and Poulin moderated. (A recording was posted on YouTube so that others could watch afterward, too.)
“What stood out to me is that we, as an organization, stepped outside of our traditional roles and became very comfortable performing tasks from other disciplines,” Poulin said.
Physical therapy doctoral student Emma George says she was surprised to learn that the dieticians couldn’t meet in person with patients in the ICU and instead had to speak with them on the phone or rely on what other team members could tell them about each patient’s condition and nutritional needs.
“I thought it was a really great experience,” George says of the mini-conference. “It was good to hear from each member of a medical care team. We talk about interprofessional collaboration in class a lot, but we haven’t really been able to see it. This was the best substitute for in-person experience that we could have.”
Jeremy Duford, a junior majoring in nutritional science, says he gained a new appreciation for both the emotional toll of working with COVID-19 patients – and the challenges of getting them to eat enough to recover.
“I knew COVID patients had no taste and no smell, but I never thought about how that would impact their nutritional recovery,” he says. “When eating is strictly a chore, it’s difficult getting those calories in. And COVID is a respiratory and throat issue, too.”
When writing a reflection paper afterward, Seeley says she realized that there is a difference between working on a team and being a team player.
“Being a team player was what these people had to do; it was like hierarchy didn’t exist,” she says. “Everyone was kind of leveled, because when it came down to it, there was one goal: Don’t get COVID, don’t spread COVID, and give your patients the treatment they deserve.”




